Advancing Therapeutic Insights: The Impact of NanoBRET® Target Engagement
Shannon Sindermann, Promega Corporation
Publication Date: April 2024
Introduction
Functional cellular and biochemical assays play a significant role in the drug discovery process, providing insight into interactions and pathways that govern cellular behavior in response to compound treatment. However, each comes with its own unique benefits and limitations. Researchers often grapple with the complex task of analyzing and interpreting the data from these two different approaches, which can be a time-consuming step in identifying the most promising clinical candidates for further advancement.
Biochemical assays are known for their quantitative, high-throughput, and target-specific nature, yet they often fall short when mimicking the complexities of living cells. Factors like cellular membrane permeability and the roles of co-factors, such as ATP, and protein:protein interactions, are not typically accounted for in these assays. On the other hand, functional cellular assays are more adept at mirroring the efficacy of compounds in vivo, frequently measuring specific downstream or phenotypic responses, but come with their own challenges including increased complexity and variability. While it is common to use both approaches at different phases in the drug discovery process, discrepancies often arise when comparing biochemical data with functional cellular outcomes. This discordance can pose significant hurdles in decision-making for the next steps in the drug development process.
A prime example of this challenge is evident in assessing the binding affinity between a compound and its target protein, a crucial parameter usually measured early in drug discovery. The strength and specificity of this interaction can be critical in driving the desired biological response. Biochemical methods are often used to quantify this compound property, allowing for rank-ordering and prioritizing compounds for further optimization. However, it is not uncommon to find that the compounds which demonstrate promising results in a biochemical affinity measure, do not produce the strongest functional cellular responses. As stated before, this disparity often stems from complexities within a cell that aren’t represented in a biochemical assay, creating a gap in our understanding.
The NanoBRET® Target Engagement Assay, or NanoBRET® TE, offers an innovative solution to this challenge. By harnessing bioluminescence and probe displacement technology, NanoBRET® TE bridges the assay divide by integrating key strengths of both biochemical and functional cellular assays into a single, scalable method. According to Matt Robers, a Senior Research Scientist at Promega, “What we have been able to do is use some of those quantitative first principles that you can see with purified protein assays, and we have ported them inside living cells.” This advancement marks a significant stride in drug discovery and identifying the most promising clinical candidates for further development.
Understanding the Functioning of NanoBRET® TE
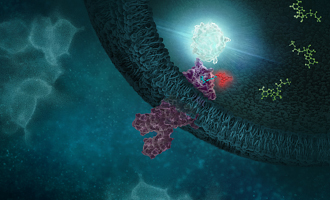
NanoBRET® TE is a cutting-edge tool designed to study the interactions of compounds, usually drug candidates, with target proteins that reside in living cells. This proximity detection assay is designed to detect the immediate proximity of two molecules by measuring the bioluminescence resonance energy transfer (BRET) from a luminescence donor to a fluorescent acceptor when they are less than 10 nanometers apart. In this process, NanoLuc® Luciferase serves as the donor and is proximal to the binding pocket on the target protein; the NanoBRET® tracer, a cell-permeable probe consisting of a fluorophore and a target binding moiety connected by a linker, acts as the acceptor.

The assay then works by expressing a NanoLuc®-tagged target of interest, which will create blue light proximal to where the target protein is expressed. Subsequently, a fluorescent drug tracer can be added to the culture medium and if a complex is formed with the NanoLuc®-tagged target, a strong BRET signal (red light) is formed, indicating a successful interaction between the tracer and the target protein. The introduction of a candidate drug molecule can compete with this tracer, influencing the red, BRET signal and providing valuable insights into molecular interactions between the drug and the target in live cells.
How to Leverage NanoBRET® TE in Research Applications
Robers emphasizes the distinctiveness of NanoBRET® TE, noting, "NanoBRET® TE stands apart from other methods because it gives you that quantitative metric and allows you to do selectivity analysis." This innovative approach makes the NanoBRET® TE assay a pivotal solution for drug discovery and enables researchers to pinpoint promising clinical candidates by accurately quantifying the drug-target interactions under a more physiologically relevant setting.
- Affinity, Occupancy and Selectivity: Quantify intracellular compound affinity, or apparent Ki, and fractional occupancy to enable precise selectivity measurements across similar targets.
- Recommended assay conditions for quantitative analysis are provided by Promega for catalog assays.
- Permeability: Assess the intracellular availability of compounds, which represents compound permeability, by comparing results of live-cell and permeabilized-cell modes.
- By using a permeable control compound, the Availability Index (AI) can be calculated, allowing compound prioritization based on permeability, an important property for high molecular weight candidates such as PROTACs.
- Residence Time: Measure compound residence time in live cells by equilibrating target-NanoLuc® fusion protein cells with a compound, then monitoring tracer binding kinetics and BRET signal production.
In addition to its primary advantages, Robers highlights that NanoBRET® TE operates without the need for cell lysis, making it “scalable into many different types of high throughput screening environments and able to run in small-scale or large-scale formats.” Furthermore, its ability to function under thermodynamic equilibrium lets the assay operate in real-time, allowing both kinetic and steady-state analysis of compound binding.
Read further to learn how NanoBRET® TE assays are being applied in real-world scenarios.
Case Study 1: Trametinib

Currently, the MAPK/ERK kinase MEK is considered a key drug target in oncology, immunotherapy and aging; however, the effectiveness of many MEK inhibitors (MEKi) is limited due to on-target toxicities and drug resistance. In a recent study at the Icahn School of Medicine at Mount Sinai, scientists sought to elucidate the unique pharmacological properties of trametinib, a MEKi and an FDA-approved drug, whose mechanism of action is not fully understood. Structural analysis using X-ray crystallography revealed that trametinib is unique among MEKi’s by engaging the interface between MEK and the pseudokinase protein KSR (kinase suppressor of RAS). In addition, structural comparisons suggest the formation of MEK/KSR complex leads to structural changes in the MEKi binding pocket, which could impact MEKi binding (1).
To validate the results from structural analysis, the researchers used NanoBRET® TE assays to measure the binding of MEKi to MEK/KSR complex within a cellular context. In agreement with the structural analysis, trametinib was unique in preferentially engaging the MEK/KSR complex, showing greater specificity. Furthermore, kinetic analysis using NanoBRET® TE assay showed prolonged residence time for trametinib. The findings suggest that trametinib's increased specificity and extended binding duration could potentially minimize side effects while continuously inhibiting MEK enzymes over a longer time span (1). This makes trametinib a targeted and enduring treatment choice, however one limitation of trametinib is susceptibility to adaptive forms of drug-resistance.
To avoid this limitation, the scientists discuss the creation of a new generation trametinib analog - Trametiglue, a molecular glue-like compound that targets the higher order protein complexes of MEK. Trametiglue possesses a sulfide group in place of trametinib’s key acetamide moiety, thus generating distinct trajectory and space-filling interactions at the KSR-MEK interface. When tested in a cellular target engagement assay, Trametiglue retained similar potency and off-rate kinetics as trametinib; however, the distinct mode of action allowed Trametiglue to exhibit improved efficacy in modulating the activity of the RAS pathway (1). Thus, showcasing a new approach for designing MEK inhibitors that could circumvent drug resistance and improve therapeutic outcomes.
In a follow-up publication, the research team at the Icahn School of Medicine at Mount Sinai extended the use of NanoBRET® TE assays to interrogate compound binding to MEK complexes in the presence or absence of the phospho-regulatory sensor 14-3-3, providing a platform to probe the complexity of the RAS-MAPK signaling pathway and to develop compounds that target specific protein complexes in this pathway. (2)
Case Study 2: PKMYT1 Kinase

Amplification of the CCNE1 locus, prevalent in various cancer types, drives high cyclin E levels that contribute to genome instability and therapeutic resistance. While directly targeting cyclin E poses challenges due to its role in normal cellular functions, leveraging a synthetic lethality approach to exploit vulnerabilities introduced by elevated cyclin E levels offers a promising therapeutic avenue for tumors with CCNE1 amplification (3,4).
In a study by Gallo et al., scientists used genome-scale CRISPR-Cas9 synthetic lethality screens to try and identify therapeutic targets for tumors characterized by CCNE1 amplification. This approach ultimately revealed a distinct susceptibility to inhibition of the PKMYT1 kinase (3). Subsequently, RP-6306, an orally bioavailable PKMYT1 inhibitor, was developed, showing significant effectiveness against CCNE1-amplified cancers, particularly when used with gemcitabine (3,4).
A critical component of this research was the NanoBRET® TE assay, which played a pivotal role in validating RP-6306's specificity and efficacy against PKMYT1. A pivotal aspect of this study was the comparative analysis of RP-6306's engagement with WEE1, another kinase with a role in cell cycle regulation, akin to PKMYT1. Through the NanoBRET® TE assay, this comparison verified RP-6306's specificity for PKMYT1, enhancing our understanding of cell cycle regulation mechanisms in cancer contexts. Moreover, the NanoBRET® TE assay facilitated the measurement of RP-6306's binding affinity to PKMYT1 within living cells, shedding light on how RP-6306 uniquely triggers premature mitosis in CCNE1-overexpressing cells by early activation of CDK1, thus disrupting DNA synthesis and leading to cell death (3,4).
Thus, synthetic lethality provides an attractive method in precision medicine for inhibition of cancer cells, while sparing normal cells. RP-6306, now in clinical trials, exemplifies synthetic lethality’s success in oncology drug discovery and offers new treatment avenues for tumors with CCNE1 amplification, and possibly for those with similar genetic alterations or transcription-driven vulnerabilities.
For additional information on the publication, read the Promega Connections blog post: CCNE1-Amplified Cancers Targeted Through Synthetic Lethality Involving PKMYT1 Kinase.
Conclusion
The NanoBRET® TE assay provides an innovative approach to the drug discovery process, merging the strengths of both functional cellular and biochemical assays. Its ability to provide quantitative insights into affinity and target occupancy of drug-protein interactions, while containing the real-life complexities of a cell, sets it apart from other techniques. NanoBRET® TE is an ideal tool for understanding mechanisms of action for potential therapeutics, validating drug targets and exploring drug selectivity and off-target effects. The research highlighted above demonstrates its critical role in paving the way for safer, more effective therapeutic candidates for challenging diseases.
References
- Khan, Z. M., et al. (2020). Structural basis for the action of the drug trametinib at KSR-bound MEK. Nature 588(7838), 509–514.
- Marsiglia, W. M., et al. (2024). Live-cell target engagement of allosteric MEKi on MEK–RAF/KSR–14-3-3 complexes. Nat. Chem. Biol. 20(3), 373–381.
- Gallo, D., et al. (2022). CCNE1 amplification is synthetic lethal with PKMYT1 kinase inhibition. Nature 604(7907), 749–756.
- Szychowski, J., et al. (2022). Discovery of an orally bioavailable and selective PKMYT1 Inhibitor, RP-6306. J. Med. Chem. 65(15), 10251–10284.
Learn more about NanoBRET® Target Engagement
Related Resources

Functional Characterization of GPCR Signaling
This webinar provides an introduction to NanoBiT® and NanoBRET® technologies for monitoring GPCR signaling.

NanoBRET® Kinase Target Engagement
In this Customer Spotlight, Dr. Gary Allenby (Aurelia Bioscience Ltd.) discusses his research using live-cell quantitative analysis of intracellular kinase target engagement.
From Hit to Live-Cell Target Engagement Assay
This blog post discusses a workflow to generate novel NanoBRET® tracers using DNA-encoded libraries (DEL).